An eating disorder is a serious illness characterized by distress regarding someone’s weight or body shape, as well as irregular eating habits. Common types of eating disorders include anorexia, bulimia and binge eating disorder.
A quick flip through a fashion magazine or a scroll through Instagram reveals pages and posts of super-thin figures that our society promotes as beautiful despite being unattainable by most people. While many people can relate to worrying about their weight or have trouble with their own body image acceptance, the most affected groups are often young women and, more recently, young men.
This obsession with the perfect body can reach an extreme level, causing abnormal eating habits that are unhealthy and even life-threatening in certain instances. When extreme food restriction or excessive exercise reaches unhealthy levels, the issue can progress into an eating disorder. Eating disorders are a type ofmental health disorder. While dangerous and life-threatening if left untreated, recovery from eating disorders is possible.
The American Psychiatric Associationlists three main types of eating disorders:bulimia nervosa,anorexia nervosaandbinge eating disorder. There are also several other less common eating disorders, as well as a category for all symptoms that don’t fall into one of the other categories, called Other Specified Feeding or Eating Disorder (OSFED). The acronym OSFED replaced Eating Disorder Not Otherwise Specified (EDNOS).
Eating disorder statisticsand research on how many people in the United States struggle with eating disorders varies. The disorders can be difficult to pinpoint and a large percentage of those affected go untreated. A dramatic overview of eating disorders comes fromThe National Association of Anorexia Nervosa and Associated Disorders. This organization states that the prevalence of eating disorders could be close to24 million people.
In addition,the Journal of Affective Disordershas reported that people who have eating disorders may also struggle with other mental health conditions. The most common co-occurring mental health condition isdepression.
Most research concludes that women are more affected than men by eating disorders, however, men do not often report having an eating disorder or seek treatment due to the stigma surrounding these conditions. No matter the most common demographics for individuals with eating disorders, these conditions cross-cultural, age and gender lines.
What Is an Eating Disorder?
Like othermental health disorders, eating disorders are often misunderstood and thought to be a choice. However, eating disorders are serious medical conditions that can be dangerous and life-threatening. Dieting does not constitute an eating disorder but may be a possible trigger.
When seeking to understand what is an eating disorder and what is not, a clear eating disorder definition can be helpful.The National Eating Disorder Association (NEDA)defines an eating disorder as a serious but treatable mental and physical illness that is characterized by distress regarding a person’s weight or body shape as well as irregular eating habits. An eating disorder can be defined by inadequate or excessive intake of food. These disorder eating patterns cause physical and mental damage.
An eating disorder can develop at any age but typically appears during the teenage or young adult stages of life. Eating disorders are treatable conditions but the consequences can be detrimental and life-threatening if they are left untreated.
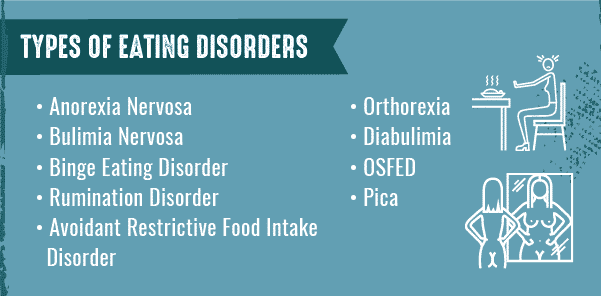
Types of Eating Disorders
While there are many different types of eating disorders, there are some that are far more prevalent than others. The most common eating disorders include anorexia, bulimia and binge eating disorder. These disorders typically involve withholding food, binge eating and purging, using different methods. There are many other eating disorders that are less common, such as pica, rumination disorder and avoidant restrictive food intake disorder.
Anorexia Nervosa
People who are diagnosed withanorexiaoften have a distorted body image and restrict the number of calories they consume in order to remain thin. Some people with anorexia may also compulsively exercise, binge eat and purge by vomiting or using laxatives. The disorder typically begins during adolescence but can occur at any age.
A common misconception about the disorder is that people who suffer from anorexia are emaciated or underweight. However, larger-bodied people and even people who are overweight may face the disorder. Additionally,atypical anorexiaoccurs when a person has all of the symptoms of anorexia but their weight remains within a normal or above the normal range.
Bulimia Nervosa
Bulimiainvolves periods of excessive overeating, known as binging, followed by purging using various methods, including self-induced vomiting or laxatives. People with bulimia have a fear of gaining weight and often have a distorted body image, but that doesn’t necessarily mean that they are underweight.
Someone with bulimia may purge to manage their current weight or to prevent additional weight gain. A person with this disorder may consume more than the recommended daily standard of 2,000 calories at once and then proceed to purge, either by vomiting, using laxatives or another method. Some of these other methods of purging may include excessive exercise or use of enemas. If someone binge eats but doesn’t purge in any form, they may have a binge eating disorder.
Binge Eating Disorder
Binge eating disorder(BED) is a serious, potentially life-threatening condition that is defined as repeated occurrences of consuming large quantities of food rapidly, to the point of discomfort. Other characteristics of BED may include feeling out of control during a binge eating episode and experiencing shame, distress or guilt afterward. This type of disorder is the most common eating disorder in America.
Pica
Picadisorder involves eating items that are not considered edible and do not contain any substantial nutritional value, like dirt, hair or cotton. Diagnosis for pica is usually made after a review of a person’s clinical history. Once a person is diagnosed with pica, additional tests may be suggested to check for anemia, potential intestinal blockages and toxic side effects of non-food items.
When determining what is pica and what is not, the intent of consuming non-food items should be considered. A person who has a fear of weight gain and eats only paper may be more likely diagnosed with anorexia. However, a person who eats dirt regularly is most likely struggling with pica disorder.
This disorder is most common in childhood. Pica is often associated with other co-occurring disorders like schizophrenia, autism spectrum disorder and intellectual disabilities. Pica is often associated with iron deficiencies or other malnutrition factors. Pica may be the body’s way of supplementing a significant nutrient deficiency.Pica treatmenttypically involves identifying the specific deficiency and supplementing nutrients to correct the deficiency.
Avoidant Restrictive Food Intake Disorder
Avoidant restrictive food intake disorder (ARFID)is a newly recognized eating disorder diagnosis. This disorder was previously known as selective eating disorder. It has been related to anorexia because both eating disorders involve limitations in the amount and types of food consumed.
However, ARFID doesn’t include any feelings of distress regarding body image, size or weight like anorexia does. ARFID is often considered an extreme form of picky eating. Some children are finicky eaters and could be diagnosed with ARFID because they don’t consume enough calories to develop and grow.
Adults can be diagnosed with ARFID as well, and in addition to not developing physically, they may have trouble with maintaining basic bodily functions. A case of ARFID may result in serious medical consequences because the body is denied essential nutrients to function and develop properly.
Rumination Disorder
Rumination disorder is an eating disorder that involves regularly regurgitating food. Once regurgitated, the food may be re-chewed, re-swallowed or spit out. Someone with rumination disorder doesn’t appear to do this purposefully. However, a person with rumination disorder is also unlikely to appear distressed, upset or disgusted by their frequent regurgitation.
Treatment for rumination disorder often includes a combination of breathing exercises and habit reversal. People who are diagnosed with rumination eating disorder are frequently taught to replace the regurgitation with deep breathing techniques.
Orthorexia
Orthorexia is a relatively new term that has not yet been widely accepted. Orthorexia nervosa is not yet a recognized eating disorder diagnosis. However, this does not mean that orthorexia is not dangerous. Defining what is orthorexia is an important step in identifying people who may be at risk for developing an eating disorder such as anorexia or ARFID.
Orthorexia is defined as an obsession with eating healthy food and avoiding unhealthy food. Because it is ultimately amental health condition, orthorexia involves far more rigid thinking patterns and eating habits than those of a person who aims to eat healthy food. A person with orthorexia is likely to experience some impairments in their life due to their obsession with healthy eating.
Diabulimia
Diabulimiais another eating disorder that is currently not well-known. Like orthorexia, diabulimia is not yet an officially recognized eating disorder. Diabulimia is a serious and potentially life-threatening condition. Understanding exactly what diabulimia is can help identify people who are struggling with this disorder and may also be at risk of developing other eating disorders. Diabulimia refers to the deliberate manipulation of insulin levels by a person with type 1 diabetes to trigger extreme weight loss. A person who induces an insulin deficiency for the purpose of weight loss can potentially develop diabetic ketoacidosis, a life-threatening medical condition.
OSFED
Other Specified Feeding or Eating Disorder, more commonly referred to asOSFED, was previously known as Eating Disorder Not Otherwise Specified (EDNOS). An OSFED eating disorder may not meet the diagnostic criteria for other eating disorders but is nonetheless serious and potentially life-threatening.In most cases, OSFED refers to a condition that has the general characteristics of anorexia or bulimia but does not meet the full diagnostic criteria for either of these conditions. For example, all criteria for anorexia may be met except for the individual’s weight not falling below the normal range. A person with an OSFED is just as likely to have serious medical consequences as individuals who fully fit an eating disorder diagnosis. Someone who has an OSFED may be just as likely to die as a result of disordered eating as anyone else with an eating disorder.
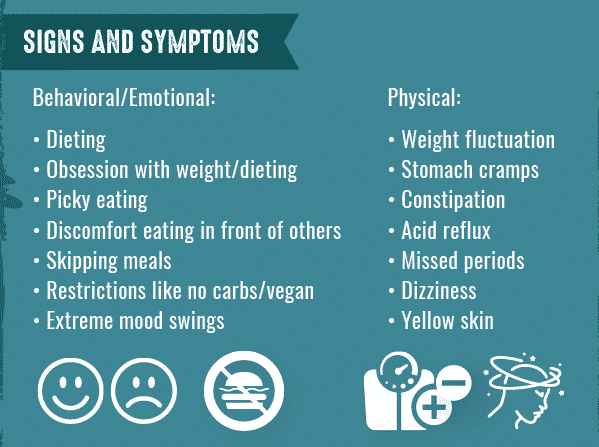
Eating Disorders Signs & Symptoms
Eating disorders may be caused by co-occurring mental health disorders and can cause physical conditions that can be life-threatening. The earlier an eating disorder is recognized, the better the chances for recovery. Recognizing the early warning signs of eating disorders can make a tremendous difference in the long-term health effects caused by the disorder. Signs and symptoms of eating disorders can be generally divided into two sub-categories: behavioral (and emotional) signs and physical signs.
Behavioral and Emotional Signs
Common emotional and behavioral signs of an eating disorder may not always be easily identifiable. Once an eating disorder is fully developed, the eating disorder symptoms will be evident. Some of the most common behavioral and emotional signs of an eating disorder include:
- Habits and practices to lose weight, including dieting and control of food intake
- Obsession with weight and dieting
- Becoming pickier about food choices
- Discomfort with eating in front of other people
- Excessive chewing to appear as if they are eating normally
- Skipping meals or taking small portions of food at regular meals
Physical Signs
Physical signs of an eating disorder may be the most dramatic of all eating disorder symptoms. Physical warning signs of an eating disorder often catch the attention of medical professionals. In situations where common behavioral and emotional symptoms are unable to be observed, a medical professional may recognize an eating disorder solely based on physical signs. Some common physical symptoms of an eating disorder include:
- Noticeable fluctuations in weight (both gains and losses)
- Stomach cramps
- Constipation
- Acid reflux
- Menstrual irregularities, including loss of periods or missed periods
- Difficulty concentrating or sustaining attention
- Dizziness or fainting, especially after standing up
- Sleeping problems
- Cuts and calluses on fingers
- Dental problems like enamel erosion, cavities and tooth sensitivity
- Dry skin, hair and nails
What Causes Eating Disorders?
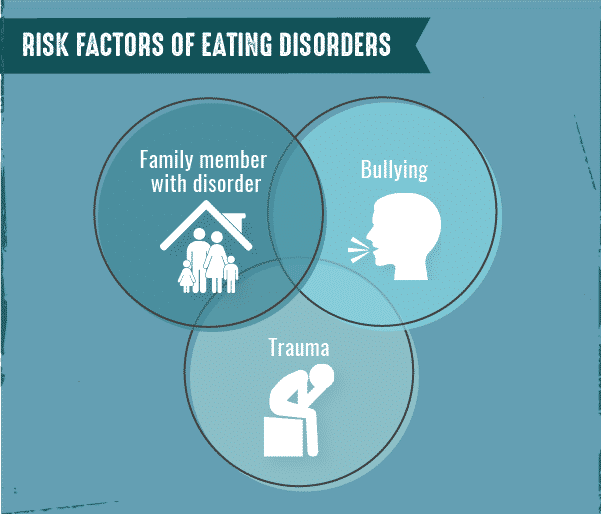
Like othermental health conditions, eating disorders are caused by a combination of environmental, genetic and social factors. While there are no factors that will definitely cause eating disorders, certain behaviors or characteristics may be predictors of eating disorders.
For example, a dysfunctional hormonal response to stress may suggest a susceptibility to developing an eating disorder. Social situations associated with sports, modeling or other occupations concentrating on body image and weight control could influence the development of eating disorders. TheNational Alliance on Mental Illnessreports that people are far more likely to develop an eating disorder if one of their immediate family members has one.
Risk Factors for Eating Disorders
Risk factors that influence eating disorders include a range of biological, psychological and socio-cultural factors. Warning signs vary from person to person, but some variables are likely to influence a person’s risk of developing an eating disorder. Some biological risk factors that are applicable to people with anorexia nervosa, bulimia nervosa or binge eating disorder include:
- Having a family member with an eating disorder
- Having a family member with another mental health disorder
Some general psychological risk factors may include:
- Perfectionism
- Body image dissatisfaction
- History of ananxiety disorder
- Rigid thinking
Some social risk factors may include:
- Weight stigma
- History of dieting
- Being teased or bullied
- Limited social networks
- History of trauma
Eating Disorders and Substance Abuse
As with other mental health disorders, eating disorders and addictions frequently co-occur. According to NEDA,up to 50 percentof individuals with eating disorders abusealcoholorillegal substances, a rate that’sfive times higherthan drug addiction rates in the general population. Additionally,up to 35 percentof people with substance use disorders also had an eating disorder.
The most common substances abused by people with an eating disorder include:
- Alcohol
- Laxatives
- Emetics
- Diuretics
- Amphetamines
- Heroin
- Cocaine
Most of these substances are known for their appetite-suppressing side effects.Dual diagnosisof eating disorders and substance abuse requires comprehensive treatment for both disorders.

Diagnosing an Eating Disorder
In most cases, patients do not ask, “Do I have an eating disorder?” Instead, diagnosis is frequently done by recognizing warning signs and then conducting further investigation to determine if an eating disorder is present. Most patients are secretive regarding their eating disorder and do not openly seek treatment.
The standard for how to diagnosis eating disorders is to follow the criteria listed within the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) for the specific disorder. There several types of professionals who can diagnose an eating disorder, and each may differ slightly in their approach. Mental health professionals like psychiatrists, psychologists and social workers, as well as pediatricians and family doctors, have the authority to diagnosis someone with an eating disorder.
Regardless of the type of professional diagnosing the eating disorder, it is common to interview the patient and ask about experience with exercise, current eating habits and their views on their weight and body image.
There is no laboratory test to screen for these types of illnesses, but professionals may use a variety of questionnaires and assessments to determine whether someone has an eating disorder. Medical doctors may use specific laboratory tests to identify possible side effects of an eating disorder.
The most common method of diagnosing eating disorders involves the use of diagnostic tools and a physical examination. These tools include blood work, a bone density exam and electrocardiogram. These eating disorder diagnosis tools indicate when a person has developed common physical conditions related to their disorder. A doctor can use this approach to determine if a person has an eating disorder and the severity of their disorder.
Treatment for Eating Disorders
Eating disorder treatment centers across the country help individuals recover from these life-threatening conditions. Eating disorder treatment may be complicated but recovery is possible. Treatment for an eating disorder is critical due to the possibility of further medical complications if the disorder continues.
Progressive treatment and therapy, including nutrition counseling and assistance for ceasing unhealthy behaviors like excessive exercise, binging and purging, are the most common types of eating disorder recovery.Integrated treatment modelsare often employed for co-occurring disorders and setback prevention.
If you or someone you know struggles with a substance use disorder and an eating disorder, help can’t wait. At The Recovery Village, we treat substance use disorders as well as co-occurring disorders, including eating disorders.Call or speak with our representativesabout enrolling in treatment start on the path to long-term recovery.
















